Sleep Disturbances as a Risk Factor for Stroke
Sleep is an indispensable part of life, as with feeding and reproduction, all animal species require sleep. Humans sleep almost one-thirds of their lifetime,which is similar in industrialized and in pre-industrial societies. Sleep, although characterized by quiescence and diminished responsiveness, is not a simple state of rest, but rather a cyclic state of periodic transitions between rapid-eye-movement (REM) and non-REM (NREM) sleep, which are precisely regulated by the central nervous system. Along with the brain and other organs or physiological streams, the cardiovascular system achieves homeostatic restoration during sleep, mainly through autonomic circulatory control. For example, the decrease in blood pressure during sleep, “dipping,” is a key biomarker of cardiovascular health, secondary to changes in activity and posture and also under the influence of sleep and circadian rhythms. During NREM sleep, the largest portion (up to 80%) of normal adult sleep, the autonomic system is stabilized with vagal dominance, reduced sympathetic tone, and heightened baroreceptor gain, contributing to a significant reduction in blood pressure and heart rate, with the greatest drop occurring during slow wave sleep. This salutatory milieu makes it easy for the cardiovascular system to maintain homeostasis
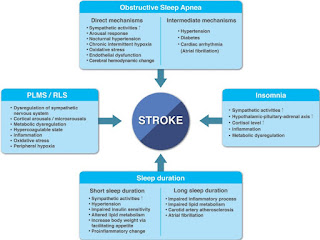
Any causes of sleep restriction, including sleep restriction, insomnia, and shift work, are likely to impair cardiovascular restoration through a reduction in cardioprotective stable NREM sleep. Sleep fragmentation, conventionally defined by cortical EEG arousals, is a universal feature of almost all sleep disorders, including sleep apnea, insomnia, periodic limb movements during sleep (PLMS) and narcolepsy, and is associated with overshoots in sympathetic activity. Even if REM sleep is preserved, the greater the sleep fragmentation, the farther the sympathovagal modulation is tilted toward sympathetic dominance . Blood pressure regulation during the biological night (the usual sleep time) is uniquely related to cardiovascular risk, including the risk of stroke. Non-dipping—loss of the typical blood pressure drop during sleep—is associated with a host of poor cardiac, neurological, metabolic, and renal outcomes. Sleep fragmentation causes non-dipping. Non-dipping is common in older adults and is associated with an increased risk of stroke. Reduced dipping is associated with brain atrophy, worse functional status, and lower daytime cerebral blood flow.
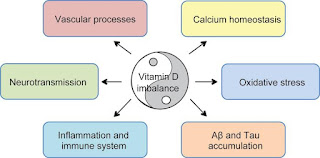
The deleterious effects of sleep disturbances go far beyond autonomic circulatory derangement. Common sleep disorders like sleep apnea, insomnia, and PLMS activate multiple mechanisms including intermittent hypoxia-reoxygenation injury, inflammation, insulin resistance, hypothalamic-pituitary-adrenal axis activation, hemodynamic swings, cardiac arrhythmia, and hypercoagulability, all of which have the potential to provoke cardiovascular diseases.


Comments
Post a Comment