Impact of Racial Differences in Alzheimer Biomarkers
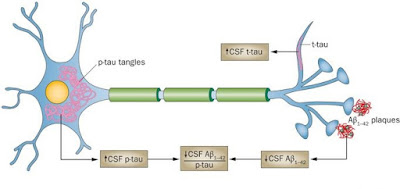
Cerebral impairment in older African
Americans is related with smaller changes in cerebrospinal fluid (CSF) tau
biomarkers but greater influence from white matter hyperintensity (WMH) burden
compared with impairment in older white Americans, according to a study from
Emory University in Atlanta, Georgia.
These race-associated
variance in CSF tau markers may result in underdiagnosis of Alzheimer disease(AD) in African Americans, according to the researchers. This is the primary
research to directly look at race, CSF AD biomarker levels, and the
relationships between WMH and cognition.
Background
The research team noted that the
occurrence of AD is nearly doubled in African Americans compared with whites.
Although African Americans also reportedly are more likely than whites to have
nonamnestic forms of mild cognitive impairment (MCI) and slower decay to and
through dementia, postmortem studies show that they have greater ischemia,
which is related with WMH burden, and Lewy body copathology.
Study
design
The Emory team assumed that CSF amyloid
biomarkers, dysfunction and neurodegeneration would differ between older black
and white Americans with normal understanding and AD-associated cerebral
impairment. They prospectively involved older black and white Americans with
either normal thought, MCI, or AD to explore race-related alterations in
efforts to improve the classification of AD and non-AD pathology in older
African Americans. A total of 66 older black and 72 older white Americans
(average age, 70 years for both cohorts) were registered in the study and
underwent detailed clinical, neuropsychological, MRI, genetic, and CSF
analyses. Aβ40 and Aβ42, tau, neurodegenerative and candidate endothelial
markers, and soluble intercellular cell adhesion molecule 1 were characterized
to test their association with cerebral impairment within each race.



Comments
Post a Comment